Understanding Clinical Need & Learning to Fail Fast: My Volunteering in the Pandemic, and a COVID-19 Ventilator That Couldn’t Save Lives
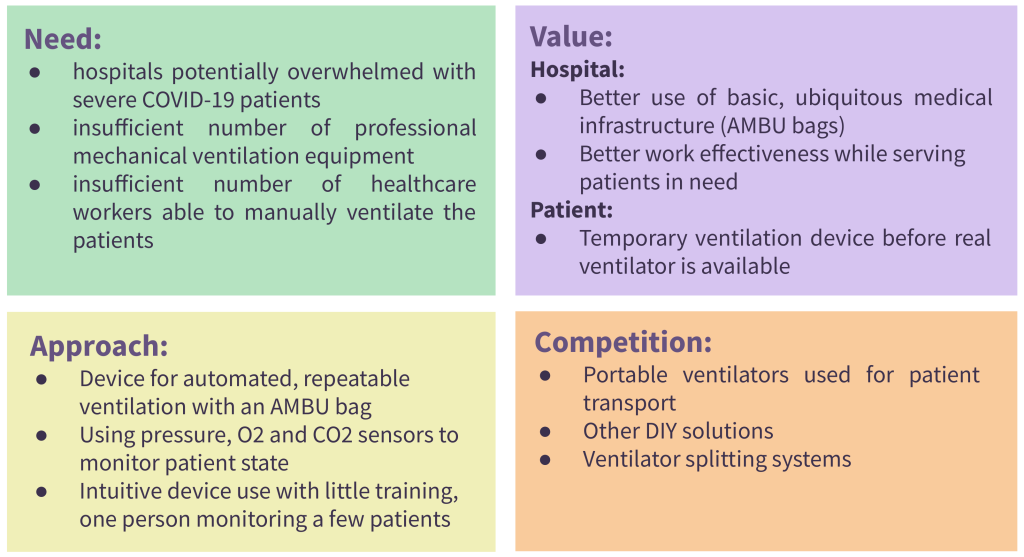
Why did I abandon my COVID-19 ventilator project soon after building the first prototype in April 2020? Why do I consider it a failure today? What did I learn? What did I do instead?
tl;dr: DIY vs. Medical-Grade Ventilation Comparison | Lessons learned and observations
The drive to be successful is fueled by stimuli from all directions. The dopamine shots of success give us a burst of energy. Typically, our self-esteem runs on achievements, just like America runs on Dunkin. But let me serve you a bitter shot of failure espresso today. Here is the story of my COVID-19 ventilator. I am going to speak out about my mistakes in pursuing this project with limited knowledge and understanding of real clinical use cases. This is also a story of how I refocused my attention, tested other ideas quickly and contributed to COVID-19 volunteering projects, which were much different and simpler than the ones I originally envisioned.
Confronting the New Reality. Extrapolating Uncertain Future.
I suddenly found myself locked down for around 6 months when visiting my homeland Poland in March 2020. Rapidly rising COVID cases were terrifying. With close friends and family I decided to challenge that new reality. How to bring the biggest value at the possibly lowest cost? How to flatten the curve, or better: enable patient recovery? I started interviewing medical doctors from the local ER (this will be important later). They were stunned and expected our healthcare system to break within 1 month – because of the ventilator shortage. But manufacturing in Poland was still up and running. So were my two 3D printers. It was the time to act. Or wasn’t it? I had some doubts. But supplied them with enough wishful thinking and sense of unprecedented urgency to move forward.
Look what is happening in Italy right now, it is soon coming to the Eastern Europe. It will happen everywhere.
The doctors in Poland worried.
I would soon dive deep into ventilation basics on the internet, and also ask my experts more questions. That would reinforce their earlier stance. Around that time I also learned about covid-19 ventilators based on a BVM (so called “AMBU” bag) that are used for manually-assisted ventilation. Moreover, there were numerous researchers and enthusiasts working on these ventilation projects. There were at least 80 different groups worldwide as of the late March 2020. These groups also developed other COVID projects – ones much less invasive as compared to ventilation. These researchers were credible, and the value proposition behind these ventilators was sound for a newbie like me. And there was one more ethical motivation.
We should try any ventilation solution that could potentially help a patient who would otherwise surely die.
None of these 80 ventilator projects could even dream of being authorized for use in regular circumstances. But it was expected that such restrictions would be lifted soon. If not by the government, then by physicians and nurses themselves – who in desperation assured me that they would use my future device.
Going Quicksilver: My Ventilator
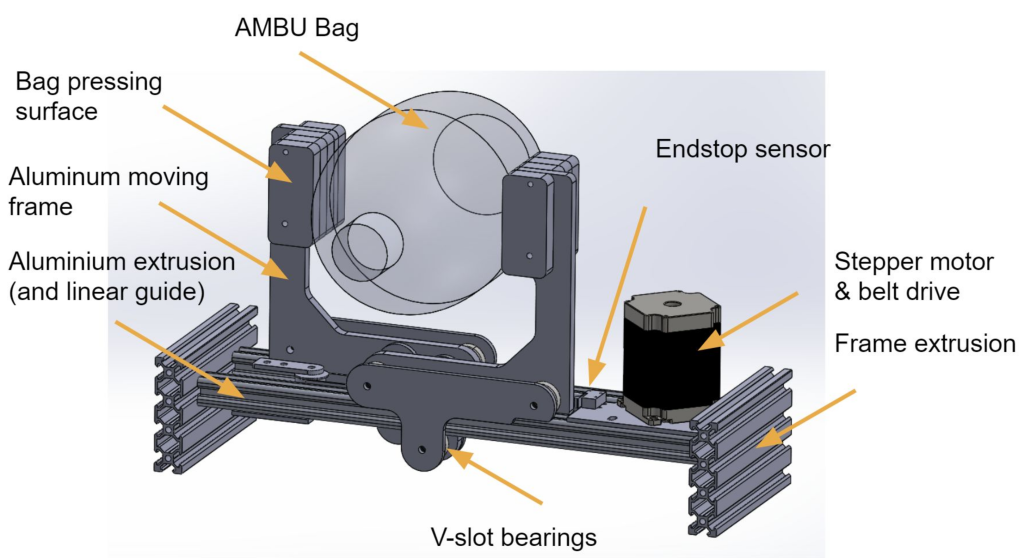
At that time, many hardware components used for high-end ventilators, like dedicated turbines or sensors were running in short supply, which was a second motivation for pushing into simpler solutions. I realized that an existing BVM would be probably the only compressible container available at scale which could be used to pump air into patient lungs and have the benefit of being cheap. The device would compress a BVM bag in a controllable manner that included variable compression range and compression speed profiles. At its output, the device would provide air reaching peak pressure, the volume of air that would be inflated to patient lungs. All of that would happen in adjustable time intervals several times per minute.
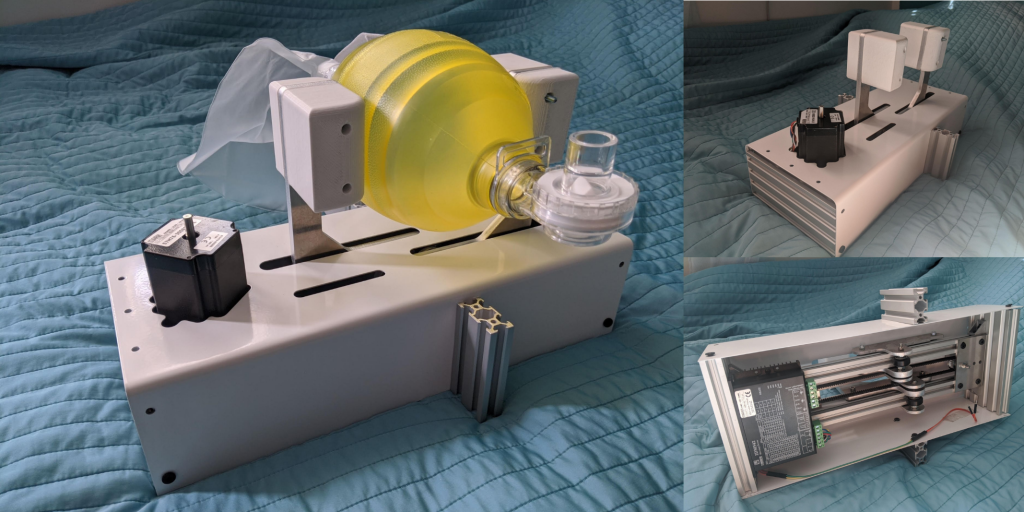
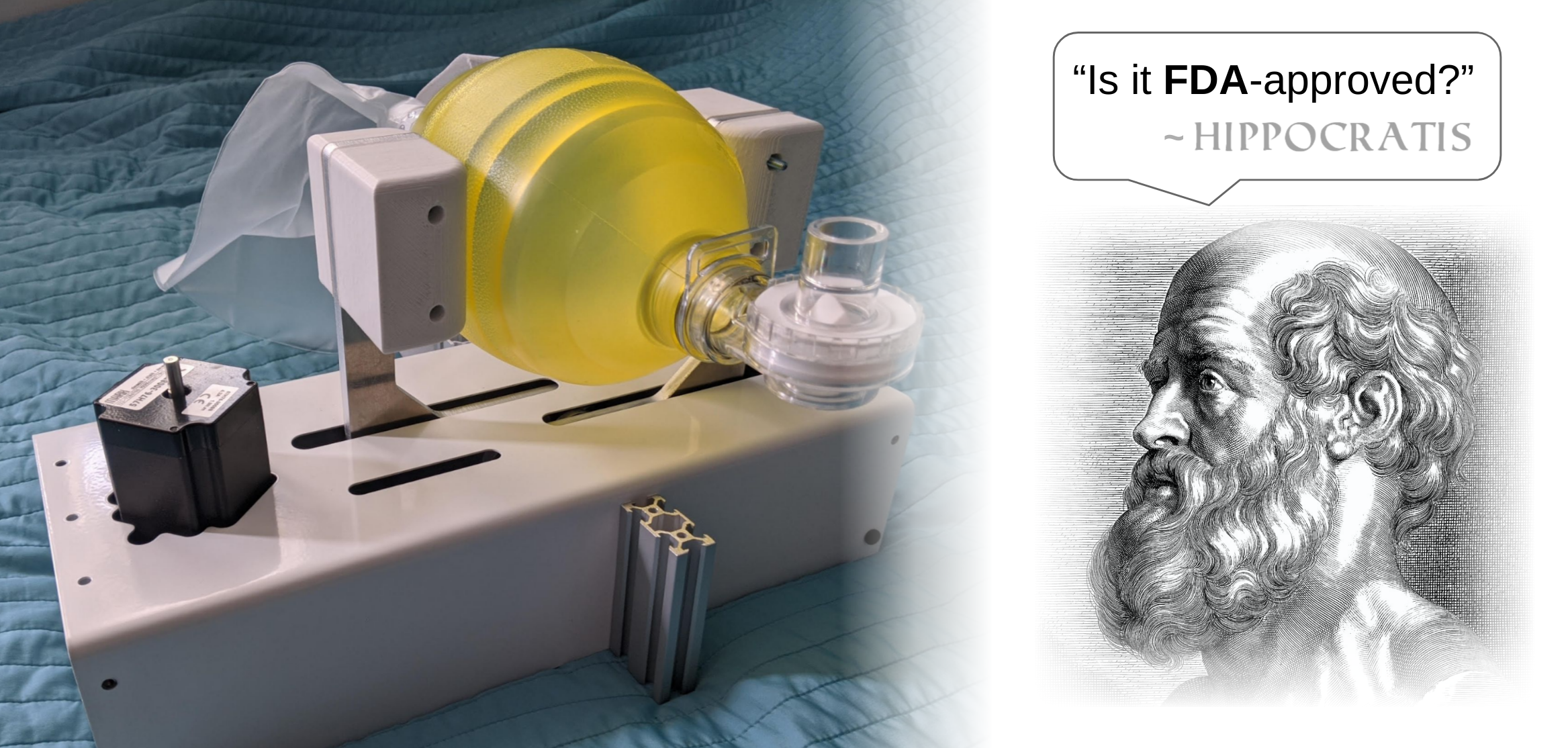
As you can imagine, there were soon 81 ventilator projects out there. For my prototype build I used aluminum extrusions, laser-cutting and sheet metal bending services, and a few 3D printed parts to get the first prototype in less than 2 weeks, all fueled by the generosity of a few companies who really cared. My device was very similar to other BVM-based projects when it comes to the general operating principles. However, at that time, the originality of my device relied on a belt drive powered by a stepper motor that moved two flat jaws that compressed BVM from the opposite sides. This way of squeezing the bag was meant to ensure symmetric bag deformation that would extend its lifespan. The power transmission of the mechanism was achieved with a reliable timing belt, and the way the device worked was expected to enable longer lifetime of a BVM bag. The design had constraints but was enough to start talks with one commercial partner interested in possible production.
Observing the landscape. Diversifying ideas. Succeeding with simple contributions.
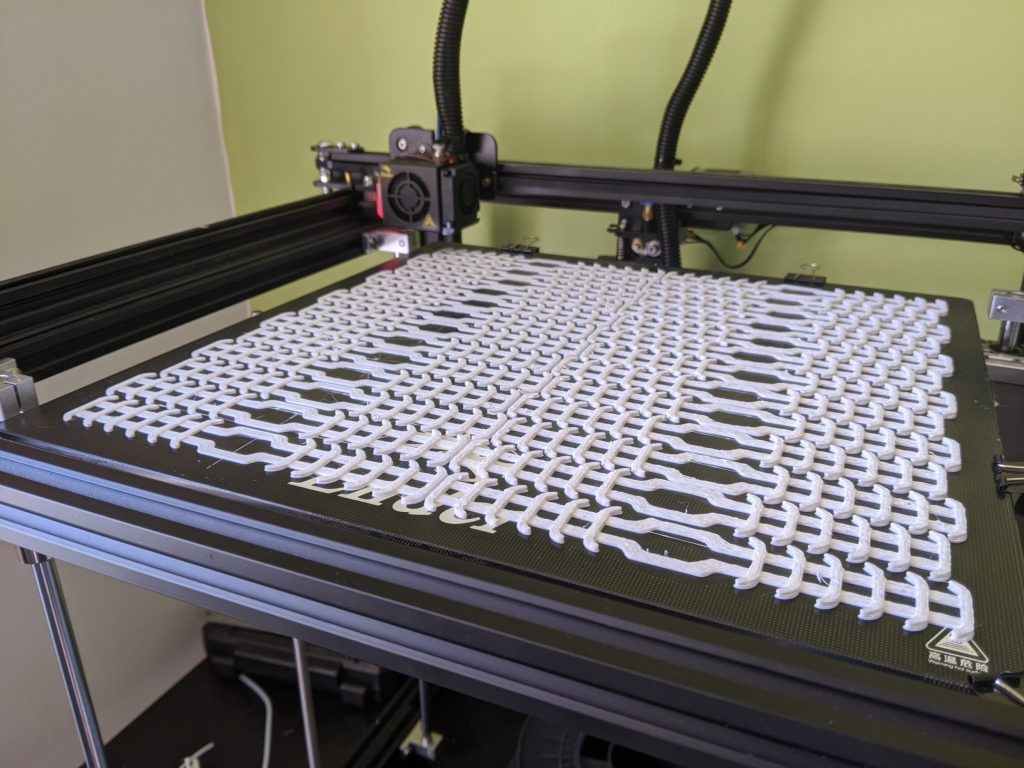
With COVID cases soaring and the potential ventilator shortage becoming even more publicly pronounced, the media turned their eyes to all these enthusiasts and geeks who were using their 3D printers and CNC machinery to produce live-saving equipment – including ventilators. Media would turn on their own “machinery” to this mix, and did a lot of positive things to promote valuable initiatives, including 3D printing which came to the mainstream even stronger – you probably saw it yourself. Many people learned about interesting 3D printing projects, like adapters for Decathlon snorkeling masks allowing the user to connect FFP3 filters and protect from the virus. Soon my 3D printers were busy manufacturing these adapters and supplying local hospitals who realized they needed them.

Independently of the ventilator project which I pursued, my friend Dariusz and I started exploring DIY ways to develop a Powered Air-Purifying Respirator (PAPR) – a personal-protective device for the head. This work was an example of moving-fast, failing-fast. We came up with a basic prototype that consisted of a construction site helmet, a piece of elastic polypropylene glass, and a trash bag. We powered this setup via a hair dryer pushing the air through a vacuum cleaner pipe. The device looked silly, but we had fun, and it worked more or less. And I really started thinking about prototypes and testing assumptions in an agile manner.

If you can answer your research question by using ready-made tools – a trash bag, a hair dryer and duct tape – use exactly these tools and nothing more. Get answers. Iterate quickly.
So what was our motivation and the research question? We wanted to quickly assess the comfort of breathing in such a mask that is nearly perfectly sealed, but has a continuous influx of fresh filtered air coming from the top. Soon we concluded that the device could offer a promising differentiation from other DIY protective gear, as it used positive pressure of filtered air to keep the virus away from spreading into the mask. However, it needed a large battery to power a turbine that could push the air through a large, potentially custom-made air filter. The device would be too much of a hassle for first responders to use it due to the bulky nature of the active pressure system and potential problems with verbal communication when wearing the device. While we could try to resolve these difficulties, there were some patents we could potentially infringe if the device was applied successfully for our pro-bono project. We did not pursue our PAPR project further.
Rather we directed our efforts more productively, in a way that would provide hospitals with supplies they needed. We worked harder on printing adaptors for virus-protecting snorkeling masks, then widely available. We could not produce our PAPR device at the scale needed, but we could provide parts for masks that were produced to scale.
Volunteering went viral
Around that time my wife Alicja has started and lead the initiative “Poznan – Szyjemy Maseczki”, “Poznan – we sew protecting masks”. In my subjective opinion, it was one of the most impactful COVID-19 initiatives in our region of Greater Poland Voivodeship. I was excited to see it growing from the very first day, when she came up with the idea to bring value by connecting people, assuming everyone would contribute to a common cause. This would soon turn out to be a great assumption.


Alicja started with a local Facebook group in our hometown Poznan and reached out to sewers, material suppliers and volunteers that would produce and distribute free protective masks for first line workers in hospitals. It was truly impressive to see this entire initiative working like a well-oiled machine. It quickly grew to a large-scale undertaking with 100 people sewing and distributing masks. They implemented strict quality and hygiene measures for producing and handling the masks and even got official mentoring and supervision from local medical authorities. They produced around 40 000 hand-made masks (which is equal to roughly 3000 hours of manual sewing). All that produced in the early months of the pandemic, when no supply chain could catch up with the production.


I mention this example to reflect on the measures of positive impact in these unprecedented times. I have seen so much joy in the eyes of people to whom I would come to deliver sewing materials or get a batch of ready protective masks. I have seen people happy to help and proud of themselves sharing their contributions with others. I realized a simple truth: that sharing these voluntary achievements with your peers is the best instant reward anyone could get out of it. It probably also kept this well-oiled machine up and running. Moreover, these contributions had a direct meaningful impact.
Volunteering went viral. There were Doers and Dreamers. I was both, and baffled. Should I aim to save future patients with magic ventilators, or make an impact here and now? What would you do?
Rising promises, rising questions
Meanwhile, companies were jumping to help and built their ventilator designs. Some of the devices were also based on a BVM bag [Virgin Orbit], others relied on the turbine-based designs [Tesla Motors], to name a few. The ad-hoc ventilator landscape started appearing to be well-explored. Seeing Corporate Social Responsibility applied to save lives is great and heartwarming – when they actually deliver on the promises.
Nevertheless, even though I was not advertising my stealth ventilator project, I was impressed how well the industry was showing their quick development. These soon-to-arrive contributions would ensure sustainable life-saving devices for all the people in need, including in the third world countries. This way of perceiving the situation further accelerated the growth of open source ventilators.
Some “Dreamers” were Self-Promoters
At that point there were a few glitches I started noticing. Some of these potential products appeared to be making too much of a good publicity – at least that was how I read unwarranted claims, fancy enclosures of simple devices inside and large company logos on these products.
Volunteering measured in likes and press releases became more pronounced.
Don’t get me wrong. Advertising products is necessary. It’s part of the usual hussle. But everything good has a limit and should be done responsibly, for instance by pointing out obvious limitations and being aware of the upcoming responsibilities. This reminded me about a venture capital advisor who once told me:
Money from venture capital comes with a contract. But it also comes with a moral responsibility: Are you ready to use someone’s pension fund for your business endeavors?
Drawing an analogy for the COVID-19 context we might ask a similar question:
Quasi-medical COVID-19 devices receive positive PR. But are their creators ready to take ownership of their promises?
Debunking false assumptions
I decided to consult more medical professionals, which was probably the best decision to take – better a few weeks late than never. I started interacting with a full-time anesthesiologist who intubated and monitored ventilated patients daily and knew high-end ventilators inside-out. I went to the ICU and observed his daily routine. I reached out to the company maintaining commercial ventilators, and they were generous enough to talk about the level of sophistication in this industry, and sent some samples of a few broken ventilator parts. I could learn from that hardware, and possibly design my own adapters for controlling the airflow or pressure measurement solutions. I also met with a biomedical engineer who trained future ventilator users. The findings were profound and a totally different reality emerged. I am going to share some of them. However, this is not medical advice.
Why did DIY ventilators fail?
First, DIY ventilators cannot effectively support actively breathing patients who occasionally make irregular breaths (spontaneous breathing). Unlike sophisticated, high-end devices, these ventilators detect such spontaneous breathing too late in the respiration cycle, and that can result with patient condition strongly worsening in a matter of hours.
Second, DIY ventilators do not enable reliable enough measurements of O2 and CO2 which could allow for ventilation process monitoring. Fine tuning of device operation characteristics is not possible either. Primarily, the oxygen concentration in the inhaled air cannot be effectively controlled or set to high levels with the devices based on BVM. The real use for BVM is only as an interim assistance.
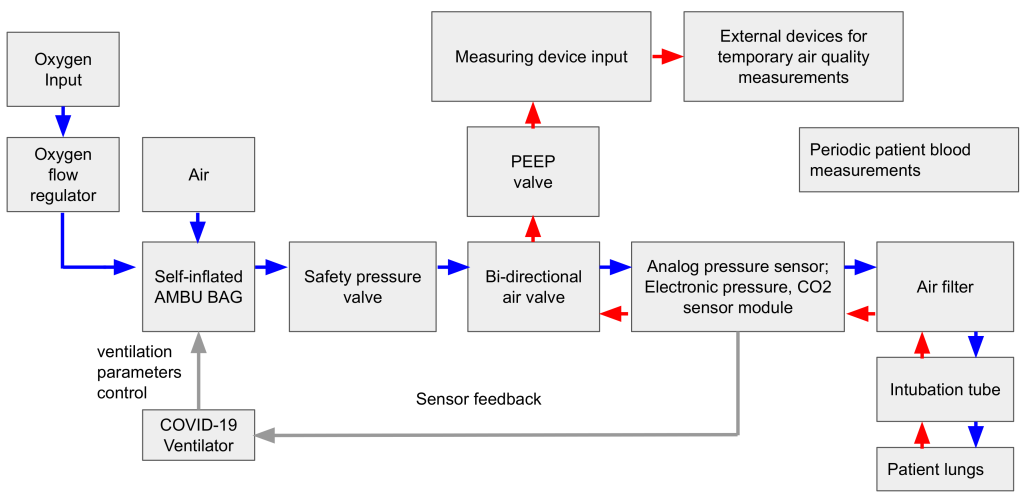
Third, the claim that DIY ventilators could save patients in low- and lower-middle income countries is inaccurate. Such regions face a scarcity of medical resources and personnel to handle difficult ventilated patients. The most severe patients are intubated and rely fully on ventilation, which means that they do not exhibit spontaneous breathing behavior – this simplifies some ventilation aspects, but other measures of patient monitoring remain challenging. The ultimate recovery from sedation is very difficult for those patients who were sedated for a prolonged time, and will be difficult to implement in the resource constrained environment. In developing countries, ventilators are not needed as much as concentrated oxygen devices, which would be a more effective means of treatment to devote resources to.
Last, but not least, the reason why DIY ventilator projects did not make it to the ICU are potential problems with production quality control, variability across devices, and the need to calibrate each unit – if the calibration was even possible. The primary problem of “Dreamers” in this pandemic was that they wanted to change the world (hopefully!) without having a know-how on producing medical devices.
The ventilator Dreamers did not know what they did not know about the medical device industry. They sprung into action and were hailed as visionary heroes. Little to no one would want to stop them. But these projects gave hope to people when the stakes were high.
The medical community that I have interacted with did not strongly scrutinize these engineering attempts in the very beginning, but rather was motivated to exhaust any option possible. If we look at it critically, it is a seemingly impossible task to succeed at producing quasi-medical devices that will provide invasive mechanical ventilation. Today, it sounds even more unrealistic to let other people make these devices in their homes and use the same control algorithm with untested sensors with an entire array of different BVM from different manufacturers.
It is one thing to showcase a device pumping air into an artificial plastic lung, and another to use it on a human.
DIY vs. Medical-Grade Ventilation Comparison
I am sure that Hippocrates would cry if he saw me advocating for the DIY ventilation cause in the early days of this endeavor. I consider my ventilator a failure, because I did not manage to identify obvious limitations of this engineering concept early enough in the design process. These limitations render the device useless for any medical purposes. I try to summarize them in the table below:
| Ventilation Task | Ad-hoc DIY invasive ventilator solutions | Medical-grade invasive ventilation solutions |
| Measuring the peak pressure in the ventilation cycle | Differential pressure sensor, safety valves | Numerous pressure sensors, failsafe mechanisms, safety valves |
| Controlling volume inflated to patient lungs | Nonlinear function of the collapsed bag and the inflated volume Difficult to control | Using a turbine with a known model, advanced flow sensors, correlating lung pressure characteristics |
| Resolving the problem of spontaneous breathing | Differential pressure sensors, detection too late in the spontaneous breathing process | Pressure sensors and devices attached to a patient signaling patient breathing intent. |
| Controlling oxygen concentration | Oxygen pipe plugged to the bag (up to 21% – 50% concentration). No accurate oxygen concentration control | Freely adjustable oxygen concentration, granular oxygen concentration control |
| Handling deeply-sedated patients | Hypothetically possible, oxygen concentration might be too low | Fully compatible with deeply sedated patients. |
| Handling lung resistance and lung compliance | peak pressure valve triggered by too-aggressive ventilation | Proprietary algorithms for on-line ventilation parameters adjustments device presets customized to patient condition |
Lessons learned and observations
DIY Ventilators shall not be forgotten
Paradoxically, despite all the reservation and practical challenges, there might be a place where the “COVID ventilators” could thrive. These devices could inspire, but not necessarily potential patient’s lungs. They could be promoting the interest in technology among many young future engineers. Making a ventilator from LEGO bricks might not save anyone today, but is a step in the direction for a good cause. I have seen ventilator projects which started with the goal of becoming life-saving tools, and ended up as educational tools for learning how a mechatronic device with several sensors and actuators works. In fact, it was for this purpose that I recently donated my own COVID ventilator.